Page content
Diabetes
Diabetes is a very complicated condition and there are many different types, but type 2 diabetes is by far the most prevalent form. Type 2 diabetes occurs when a person’s blood glucose levels are too high, because of the body is not producing enough insulin, or if the insulin produced is not effective.
Chronic elevation of blood glucose levels is very serious and can lead to damage to many parts of the body, including eyes, heart, kidney and feet. There is currently no cure for type 2 diabetes, so it is imperative that we have safe and effective medications to help maintain appropriate blood glucose levels throughout life.
Thankfully we have medicines that can help control blood glucose levels. However, we know from experience that these medications tend to fail over time, and those living with type 2 diabetes often require multiple medicines to achieve adequate blood glucose control. Unfortunately, at times even this is not sufficient, and it is therefore essential to develop new drugs to help manage the disease more effectively.
We are addressing this need though generation, testing and publicising our new safe and effective peptide-based therapeutics for type 2 diabetes.
Our approach
We make use of naturally occurring peptide hormones that are released by the body to control blood glucose levels, but do not seem to work as well as predicted in people living with type 2 diabetes. We use peptide chemistry knowledge to design new molecules that replicate the action of these naturally occurring peptide hormones, but are more powerful and longer acting. In this way, we aim to overcome the lack of biological effect of these molecules that is observed in type 2 diabetes.
Since we are using compounds that are based on naturally occurring molecules found within the body, this helps to reduce adverse effects often associated with other drugs. Moreover, this approach has been adopted for some of the currently approved drugs that are prescribed for type 2 diabetes, confirming applicability of our approach.
Use of animal models
As we progress this work towards clinical trials for type 2 diabetes, it is necessary to validate that our novel compounds are both effective and safe. Since type 2 diabetes in humans is highly complex, the human disease is unable to be fully replicated in a single animal model. We therefore make use of animal models that develop diabetes from either consuming a high calorie diet OR have a genetic mutation that leads to diabetes OR we make use of drugs that damage insulin secreting cells in the animal’s body. We have used animal models to demonstrate the effectiveness and safety of new peptide hormone drugs.
We have also demonstrated that our novel drugs can lead to positive disease-modifying benefits where insulin secreting cells in the body are renewed and/or protected from damage (Figure 1). We have further shown that application of our approach to the treatment of diabetes in these animal models results in dramatic improvements in diabetic status.
We fully appreciate that some people have concerns about the use of animals in medical research. However, this research can and has provided important, contributing to improvements to the lives of people currently living with diabetes across the world. Many people with diabetes would not be leading the lives they are today if the major advances in understanding and treating diabetes had not been made through this research, some of which must involve use of animals to ensure validity of findings.
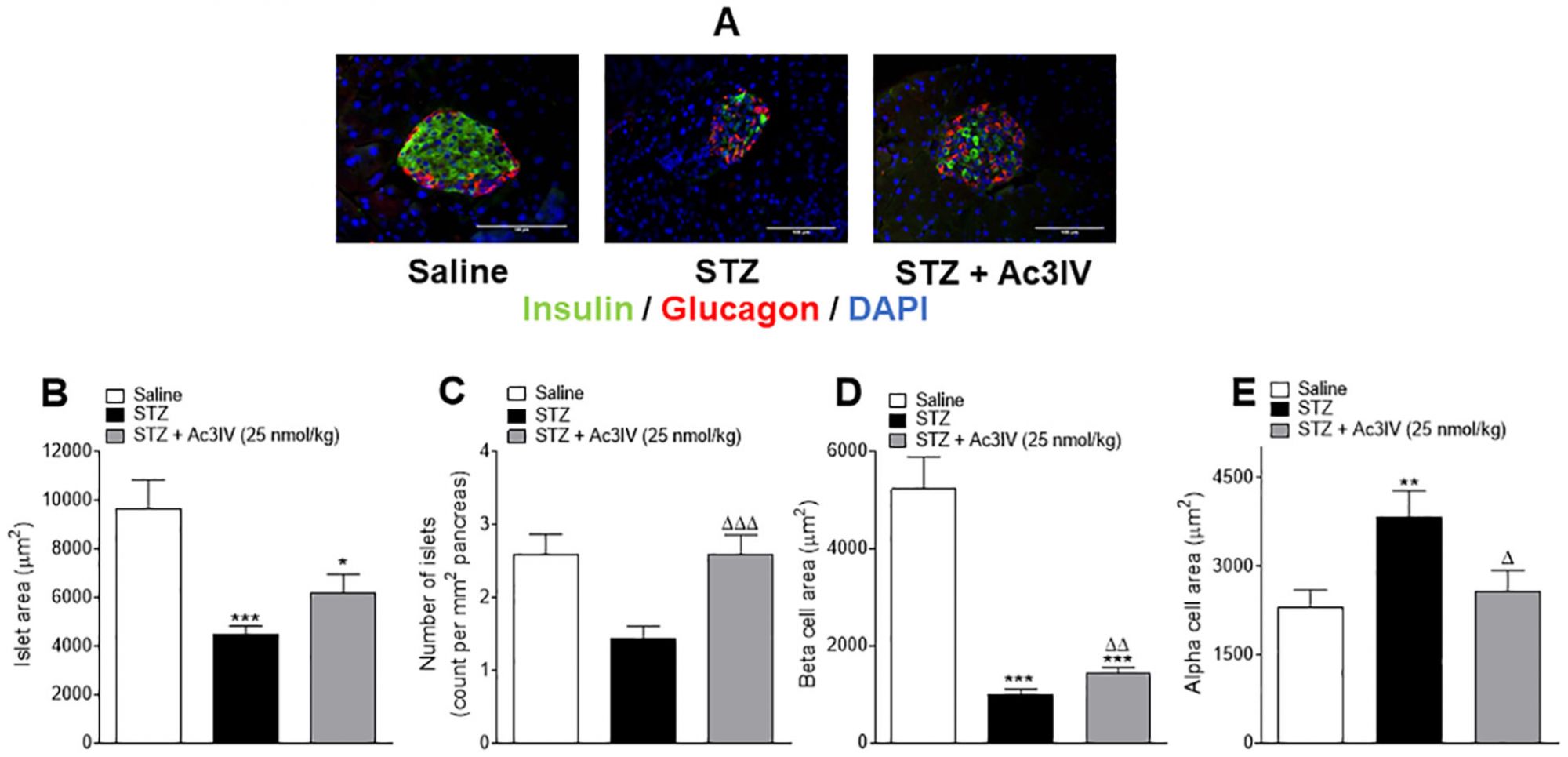
This Figure demonstrates that a long-acting peptide analogue of arginine-vasopressin, namely Ac3IV, has disease-modifying effects to correct aspects of pancreatic histology in mice with streptozotocin (STZ)-induced insulin deficiency and diabetes.
These parameters were assessed following 12 days of twice-daily treatment with saline (0.9% NaCl) vehicle or Ac3IV (25 nmol/kg bw, i.p.) in STZ-diabetic mice. Representative images (40X) of stained islets are provided in panel (A). Islet area (B) number of islets/mm2 of pancreas (C), beta- (D) and alpha-cell areas (E) were assessed using CellF imaging software and the closed loop polygon tool.
Values are mean ± SEM for n = 6 mice. *p<0.05, **p<0.01, ***p<0.001 compared to saline vehicle. Δp<0.05, ΔΔp<0.01, ΔΔΔp<0.001 compared to STZ-diabetic controls mice.

















