About the project
The project will develop and evaluate a novel integrated primary care and community-based programme to treat obesity, the first service model in Northern Ireland, whilst in ROI it will seek to build on existing obesity services.
The programme has been jointly developed by healthcare professionals with experience in treating obesity, academics, and patients living with obesity.
Our integrated cross-border multidisciplinary team will deliver specialist obesity care to 9000 people in rural and urban communities within Derry-Londonderry, Strabane, Limavady and Donegal.
The effectiveness of the model will be assessed in how it improves patients’ quality of life and key clinical measures of health, as well as its acceptability to patients and healthcare staff.

A PeacePlus project
The project is supported by PEACEPLUS, a programme managed by the Special EU Programmes Body (SEUPB) through provision of a grant up to €9,915,255.

The challenge
Approximately 1.2 million people live with overweight or obesity in Northern Ireland and the border counties of Ireland and by 2035 this number is projected to be 2.1 million if prevention and treatment do not become more effective (DoH NI 2023; DoH 2023; HSE 2021).
Currently, the management of obesity is a major unmet need. This unmet need is even more critical in the Northwest as a region of heightened deprivation (IJpelaar et al. 2018) and transgenerational trauma (Long 2021) where a lack of access to equitable health fosters division and exclusion (Percival et al. 2023).
There are no specialist obesity management services in primary or secondary care in Northern Ireland, whilst in the Republic of Ireland service provision is not optimal.
Obesity causes suffering to the individual and poses a major financial burden to the healthcare system and society.
The health complications of obesity and the current inequitable access to care, threaten the prosperity of local communities, are a barrier to them reaching their full potential.
Our goals
The PEACETIME project aims to address the significant negative impact of the chronic disease of obesity on people, healthcare systems and societies.
The objective of PEACETIME is the development and evaluation of a novel integrated cross-border clinical service that will increase access to care for people living with obesity.
The clinical model will be based on existing primary care and community structures, thereby ensuring equitable access to health care and fostering resilience of the healthcare system in the North West of Ireland.
The clinical programme
The ethos underpinning PEACETIME is that obesity is a chronic disease that responds to chronic multidisciplinary treatment.
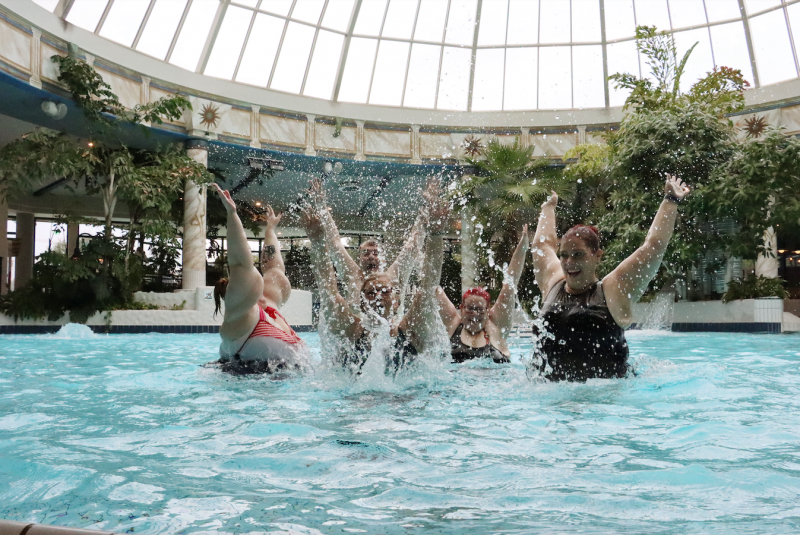
There will be a strong emphasis on quality of life, mental health, person empowerment and self-management.
Patients will undergo a 12-month obesity treatment programme, which will be nurse-led and delivered by a multidisciplinary team.
Patients will receive nutritional, psychological, physical activity, pharmacological and health coaching therapies.
The programme will be personalised to the meet the specific needs and disease complexity of the individual, with a combination of 1:1, group and online sessions supported by an e-health platform to increase reach and sustainability.
Expected changes
Change to people living with obesity
- Better access to multidisciplinary obesity care for 9000 people leading to improvements in quality of life, physical and psychological health.
Change to the healthcare service
- Reduction in healthcare costs.
- Reduction in healthcare inequalities by ensuring equitable access to obesity care.
- Fostering resilience of the local healthcare systems by moving obesity care from the hospital to the community and maximising digital healthcare.
Change to local society
- Reduction in societal costs of obesity.
- Fostering of social cohesion.
- Empowerment of communities to reach their full potential,
Change to scientific knowledge
- Generation of new evidence regarding the effectiveness of our novel primary care/ community based programme for obesity using qualitative methodologies and health economics.
- Generation of evidence regarding novel nutritional, digital/wearable technology, health coaching programmes for obesity, predictors of response to treatment and data analytics.
Partners
Ulster University
Ulster University is a multi-campus public university located in Northern Ireland.
We are a research-intensive university, creating research that impacts society and the economy, focused on developing inquiring minds and building sustainable futures for all.
We are in the Top 10% of UK Universities for outstanding (4*) or very considerable (3*) research impact.
We were awarded ‘University of the Year 2024’ by Times Higher Education.

Atlantic Technological University
ATU is a multi-campus technological university in the west and northwest of Ireland that delivers a rich combination of academic and research excellence, quality of life and opportunity.
Our collaborative ethos drives us to deliver practical, solution-oriented education and research that directly addresses global challenges.
Irish Coalition for People Living with Obesity (ICPO)
ICPO are a volunteer non-profit patient led organisation.
Their mission, as a group of people living with obesity, is to provide or direct people to education, support and raise awareness for people living with overweight or obesity across Ireland.

Derry GP Federation
The Derry GP Federation is one of 17 Federations covering Northern Ireland, it brings together 27 practices across Derry/Strabane and Limavady united by a shared commitment to work collaboratively.
Established as a Community Interest Company, it aims to improve health and well-being by delivering patient-centred care. Serving as a strong voice for primary care in the West, the Federation helps shape health and social care transformation.
Through partnerships with health, social care, and other agencies, the Federation develops services tailored to local needs while enabling large-scale commissioning across towns and districts, ensuring responsive, accessible, and better care for patients.

National Institute for Prevention and Cardiovascular Health (NIPC)
The National Institute for Prevention and Cardiovascular Health (NIPC) is an independent, not-for-profit institute for medical research and education co-founded in 2014 by the University of Galway and Croí, the Heart and Stroke Charity.
It is dedicated to a life-course approach to the prevention of cardiovascular disease and advancing cardiovascular health for all through high-quality translational research, accredited education and training, and the integration of evidence-based outcomes into policy and practice.
With a strong regional, national and international presence, NIPC plays a leading role in advancing the early detection and prevention of cardiovascular disease in line with global best clinical practices.
NIPC is committed to excellence, collaboration and innovation, working across sectors and borders to deliver measurable impact and long-term improvements in cardiovascular care, healthcare delivery and cardiovascular health policy.

Associate Partners
Northern Ireland
- Department of Health (Digital Health and Care NI)
- Derry City and Strabane District Council (DCSDC)
- Developing Healthy Communities Northern Ireland (DHC)
- Diabetes UK Northern Ireland
- European Association for the Study of Obesity (EASO)
- Royal College of General Practitioners Northern Ireland (RCGPNI)
- UK Association for the Study of Obesity (ASO)
Republic of Ireland
- Association for the Study of Obesity Ireland (ASOI)
- Diabetes in General Practice (DiGP) Republic of Ireland
- Diabetes Ireland
- HSE National Clinical Programme for Diabetes
- HSE National Clinical Programme for Obesity
- Inishowen Development Partnership (IDP) ATU
- Irish College of General Practitioners (ICGP)
- Irish Endocrine Society (IES)
- Leitrim County Council
- University College Dublin (UCD)
- Western Development Commission (WDC)